Oral Dysbiosis The imbalance between the host and microbiota disrupts microbial diversity, reducing beneficial bacteria and allowing harmful pathogens to thrive. This weakens immune defense, leading to oral diseases like dental caries and periodontal disease, causing tissue and tooth damage.
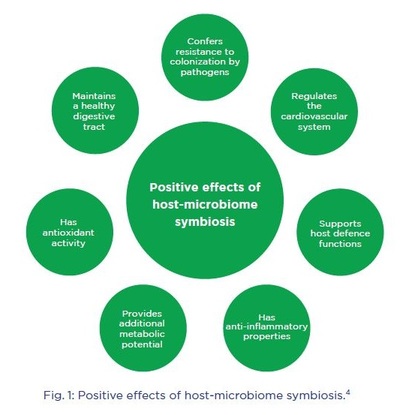
Role of Oral Microbiota in Oral Health: The oral cavity supports microbiota due to its warm, moist, nutrient-rich environment. Early colonizers include Gram-positive Streptococci and Actinomyces, adhering to surfaces and forming biofilms. In a healthy state (eubiosis), a symbiotic balance exists. However, this can shift to dysbiosis, marked by altered bacterial metabolism and linked to periodontal disease, disrupting the oral ecosystem's balance.

SYMPTOMS
Dental Caries:
Dental caries driven by bacterial pathogens and characterized by progressive dental hard tissue deterioration. The caries biofilm, a complex and highly active ecosystem, initiates the accumulation of dental plaque on the tooth’s surface. Within this environment, various microorganisms colonize, with S. mitis and S. mutans being among the initial colonizers. The formation of the biofilm begins when a salivary glycoprotein film (dental pellicle) coats a tooth surface.

Gum Swelling:
Dental caries driven by bacterial pathogens and characterized by progressive dental hard tissue deterioration. The caries biofilm, a complex and highly active ecosystem, initiates the accumulation of dental plaque on the tooth’s surface. Within this environment, various microorganisms colonize, with S. mitis and S. mutans being among the initial colonizers. The formation of the biofilm begins when a salivary glycoprotein film (dental pellicle) coats a tooth surface.
Gingivitis:
Gingivitis is gum inflammation caused by plaque buildup from poor brushing. Effective brushing removes debris and prevents plaque growth. Bacteria in plaque can infect the gingival sulcus, leading to infection. Common microbes include P. gingivalis, A. actinomycetemcomitans, and others. If untreated, gingivitis may progress to periodontitis, causing irreversible damage to gums and bone.

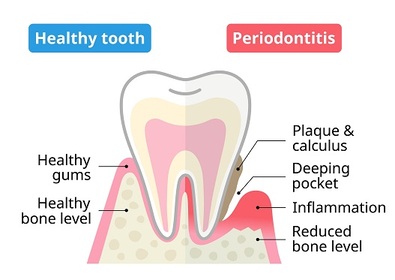
Periodontitis:
Dental plaque bacteria are key in periodontal disease, forming biofilms in supragingival and subgingival areas. The red complex (P. gingivalis, T. denticola, T. forsythia) disrupts host balance, causing bone loss. Periodontitis may also increase risk for systemic diseases like CVD, diabetes, and cancer. Interestingly, S. mutans, a major caries pathogen, shows a negative correlation with key periodontitis pathogens.

Halitosis:
Halitosis, commonly referred to as oral malodor or bad breath, is a frequent oral condition marked by an unpleasing or disagreeable odor that originates within an individual’s mouth. Gram-negative bacteria, including Prevotella (Bacteroides) melaninogenica, Treponema denticola, Porphyromonas gingivalis, Porphyromonas endodontalis, and others like Enterobacteriaceae, Tannerella forsythia, Eikenella corrodens, and various Fusobacterium species, are implicated as likely contributors to oral malodor
Tooth decay:
Tooth decay (caries) is caused by acid-producing bacteria that break down tooth tissue, forming cavities. Symptoms include pain and eating difficulty; complications include infection and tooth loss. Sugary diets, low saliva (from diabetes, Sjögren’s, or medications), poor oral hygiene, and poverty increase risk. Research into stem cell-based tooth regeneration is ongoing, though current treatments focus on managing symptoms.